Rheumatoid arthritis
In Vietnam, the rate of people with rheumatoid arthritis is 0.5%, accounting for 20% of people with joint diseases treated in hospitals. Rheumatoid arthritis not only affects daily life but also affects the ability to study and work. The following article provides you with the necessary information about this disease.

Rheumatoid arthritis is a disease in which the immune system attacks the joints, leading to joint pain, stiffness and swelling, and joint destruction.
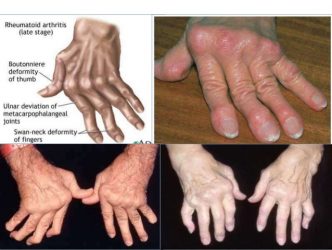
The disease causes joint pain, stiffness, and swelling in the joints. In some people, rheumatoid arthritis also causes joint damage and deformity.
Although rheumatoid arthritis affects all joints in the body, it is commonly found in the following joints: hands, wrists, feet, knees and is symmetrical.
Sometimes, rheumatoid arthritis can affect other parts of the body besides the joints, such as the heart, lungs, eyes, and mouth.
Rheumatoid arthritis lasts for several years or a lifetime and treatment lasts for several months or years.
Causes of rheumatoid arthritis:
The cause of rheumatoid arthritis has not been found yet, many scientists believe that rheumatoid arthritis is related to genetic factors.
Who is at risk for rheumatoid arthritis?
Rheumatoid arthritis is less common than other joint diseases.
About 1 million people in the United States have rheumatoid arthritis.
Women are more likely to get this disease than men, about 7/10 people with rheumatoid arthritis are women.
Although rheumatoid arthritis can occur in anyone, it is most commonly seen in people between the ages of 30 and 50.
Clinical symptoms of rheumatoid arthritis
Onset: 85% start slowly, gradually increasing, 15% suddenly with signs of acute inflammation; most are monoarthritis, which is one of the joints of the hand (wrist, metacarpophalangeal, proximal finger), knee. Lasts from several weeks to several months and then moves to the full-blown stage.
General: Polyarthritis.
Location: Early is the joints in the limbs, dominant at the distal root.
Upper limb: Wrist, fingers, closest fingers are 2nd and 3rd fingers.
Lower limbs: Knees, ankles, metatarsals and toes.
Late are the joints: elbow, shoulder, hip, cervical vertebrae, temporomandibular, sternoclavicular.
Properties: Tendency to spread to both sides and symmetry:
Swelling, pain and limited mobility, little redness, there may be fluid in the knee joint.
Pain increases at night and early morning, stiffness in the morning.
The fingers are diamond shaped, especially fingers 2 and 3.
Characteristic joint deformities appear more slowly: wind-blown hand, camel-back hand.
Extra-articular symptoms
Whole body: Mild fever, pale skin, poor sleep and appetite, weight loss, autonomic nervous system disorder.
Paraarticular manifestations:
Subcutaneous nodules: Raised above the skin surface, firm, painless, d: 0.5-2cm, commonly found on the ulna near the elbow joint, on the tibia near the knee joint, number from one to several nodules.
Dry skin, swelling of a limb, erythema of the palms.
Muscle atrophy: obvious in the area around the inflamed joint, tendinitis: often occurs in the Achilles tendon.
Very rare in clinical practice:
Heart: Occult myocardial damage, possible pericarditis.
Lungs: Mild pleurisy, alveolar fibrosis.
Spleen: splenomegaly and leukopenia in Felty syndrome
Bones: calcium loss, spontaneous fracture.
There are also: keratitis, iritis, compression of peripheral nerves, hypochromic anemia, autonomic nervous system disorders, Amyloid infection mainly manifested in the kidneys, often appearing very late.
Diagnosis of rheumatoid arthritis
American College of Rheumatology (ACR) 1987 criteria
Currently, this standard is still the most widely applied in the world and Vietnam for the manifestation of multiple joints and the duration of arthritis over 6 weeks.
+ Morning stiffness lasting more than 1 hour
+ Inflammation of at least 3 joint groups: soft tissue swelling or effusion in at least 3 of the following 14 joint groups (including both sides): proximal interphalangeal joints, metacarpophalangeal joints, wrist joints, elbow joints, knee joints, ankle joints, metatarsophalangeal joints.
+ Arthritis of the hands: swelling of at least one group of the wrist joints, proximal interphalangeal joints, and metacarpophalangeal joints.
+ Symmetrical arthritis.
+ Subcutaneous nodules.
+ Positive serum rheumatoid factor
+ Typical X-ray signs of RA: X-ray of the hand, wrist or damaged joint: erosion, cavity, bone head defect, joint space narrowing, bone head mineral loss.
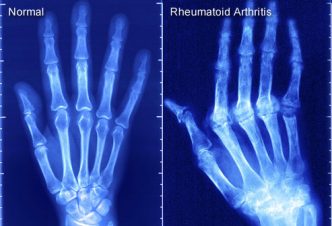
Definitive diagnosis : when there are ≥ 4 criteria. Arthritis symptoms (criteria 1-4) must last ≥ 6 weeks and be determined by a physician. The 1987 ACR criteria have a sensitivity of 91-94% and a specificity of 89% in patients with advanced RA. In the early stages of the disease, the sensitivity ranges from 40-90% and the specificity from 50-90%.
Note: Subcutaneous nodules are rare in Vietnam. In addition, it is necessary to examine extra-articular symptoms such as: muscle atrophy, iritis, pericardial effusion, pleural effusion, vasculitis... which are often rare, mild, and easily overlooked.
American College of Rheumatology/European League Against Rheumatism 2010 (ACR/EULAR 2010) criteria . This criterion can be applied in cases of early stage disease, joints inflamed for less than 6 weeks and oligoarticular type. However, it is necessary to always monitor and re-evaluate the diagnosis because in many cases this can also be an early manifestation of another joint disease other than rheumatoid arthritis.
Treatment of rheumatoid arthritis symptoms: to improve inflammation, reduce pain, and maintain mobility (however, these drugs do not change the progression of the disease).
– Non-steroidal anti-inflammatory drugs (NSAIDs).
+ Selective COX2 inhibitor anti-inflammatory drugs (first choice because they often require long-term use and have few adverse interactions with methotrexate)
Celecoxib: 200 mg, taken 1 to 2 times daily.
Or Meloxicam: 15 mg intramuscularly or orally once daily.
Or Etoricoxib: 60 – 90 mg, taken once daily.
+ Non-selective anti-inflammatory drugs
Diclofenac: oral or intramuscular injection: 75 mg x 2 times/day for 3 – 7 days. Then oral: 50 mg x 2 – 3 times/day for 4 – 6 weeks.
Brexin (piroxicam + cyclodextrin) 20mg daily oral
+ Or other non-steroidal anti-inflammatory drugs (equivalent dose).
Note : when used for patients with risk factors for unwanted effects of KVKS drugs (NSAIDs) (elderly patients, history (previous history) of stomach disease...) or long-term treatment, it is necessary to monitor kidney function and protect the stomach with proton pump inhibitors.
– Corticosteroids (Prednisolone, Prednisone, Methylprednisolone)
+ Usually used short-term while waiting for basic treatment drugs to take effect. Indicated when there is a progressive episode (criteria for a progressive episode see Appendix)
+ Moderate: 16-32 mg methylprednisolone (or equivalent), taken daily at 8 am, after meals.
+ Severe: 40 mg methylprednisolone IV daily.
+ Acute, severe, life-threatening progression (vasculitis, severe extra-articular manifestations): start with 500-1,000mg of methylprednisolone IV infusion for 30-45 minutes/day, treatment for 3 consecutive days. Then switch back to the usual dose. This regimen can be repeated every month if necessary.
+ Long-term use (usually in severe patients, corticoid dependent or with adrenal insufficiency due to prolonged corticoid use): start at an oral dose of 20 mg daily, at 8 am. When clinical and laboratory response is achieved, gradually reduce the dose, maintain the lowest dose (5 - 8 mg daily or every other day) or stop (if possible) when the basic treatment is effective (after 6-8 weeks).
Basic treatment with disease-modifying anti-rheumatic drugs (DMARDs) to slow or stop disease progression requires long-term treatment and monitoring of clinical and paraclinical symptoms throughout the treatment period.
– New and common forms: use classic DMARDs
+ Methotrexate starts at 10 mg once a week. Depending on the response, maintain a higher or lower dose (7.5 – 15 mg) per week (maximum dose is 20 mg/week)
+ Or Sulfasalazine starting at 500 mg/day, increasing by 500 mg per week, maintaining at a dose of 1,000 mg x 2 times per day
+ Combination: methotrexate with sulfasalazine or hydroxychloroquine if monotherapy is ineffective
+ Combination: methotrexate, sulfasalazine and hydroxychloroquine if the above combination is not effective
– Severe, resistant to classic DMARDs (no response after 6 months) requires combination with biological drugs (biological DMARDs)
+ Before prescribing biological drugs, it is necessary to do tests to screen for tuberculosis, hepatitis, liver and kidney function tests and assess the level of disease activity (erythrocyte sedimentation rate or CRP, DAS 28, HAQ).
+ Combination of methotrexate and anti-Interleukin 6 drug (tocilizumab)
Methotrexate 10 – 15 mg per week + tocilizumab 4 – 8 mg/kg body weight, equivalent to 200 – 400 mg IV once a month.
+ Or combine methotrexate and one of the following 3 anti-TNFα drugs:
Methotrexate 10-15 mg weekly + etanercept 50 mg subcutaneously once weekly.
Methotrexate 10-15mg weekly + infliximab IV 2-3mg/kg every 4 – 8 weeks.
Methotrexate 10-15mg weekly + adalimumab 40mg subcutaneously every 2 weeks
+ Or a combination of methotrexate and anti-B lymphoblastic drugs (rituximab)
Methotrexate 10 – 15 mg per week + rituximab IV 500 – 1000 mg x 2 times, 2 weeks apart, can repeat one or two courses per year
+ After 3-6 months of treatment, if the first biological drug is not effective, a second biological drug can be considered. Similarly, a third biological drug can be considered if after 3-6 months, the second biological drug is not effective.
Other combination treatments
– Support measures
+ Exercise and guide movements to prevent tendon contraction, joint adhesion, and muscle atrophy. During acute inflammation: let the joint rest in a functional position, avoid placing or padding the joint. Encourage exercise as soon as inflammation symptoms subside, gradually increase, exercise many times a day, both actively and passively according to the physiological function of the joint.
+ Rehabilitation, physical therapy, mineral baths, orthopedic surgery (bone cutting, axis correction, artificial joint replacement when indicated).
– Prevention and treatment of complications of treatment and associated diseases
+ Gastritis and duodenal ulcers: need to be proactively detected and treated because over 80% of patients have no clinical symptoms.
+ Prevention (when there are risk factors) and treatment with proton pump inhibitors, along with drugs to treat Helicobacter Pylori (if there is HP infection).
+ When using any dose of corticosteroids for more than 1 month, calcium and vitamin D supplements are needed to prevent osteoporosis. If the patient is at high risk of osteoporosis, bisphosphonates can be used. When osteoporosis is present, appropriate drugs (usually bisphosphonates) should be selected depending on the degree of osteoporosis, age, gender and specific conditions of the patient.
+ Anemia: folic acid, iron, vitamin B12…
Above is the necessary information about rheumatoid arthritis that you can refer to. Prolonged rheumatoid arthritis leads to destruction and deformation of joints, so when experiencing any symptoms of joints: swelling, pain, stiffness, you should go to the nearest medical facility for examination and treatment.
(References: INH, internal medicine and treatment, Advances in the medical treatment of rheumatoid arthritis, Advances in rheumatology: new targeted therapeutics)