Things you should know about rectal cancer
Colorectal cancer is the second leading cause of cancer deaths (after lung cancer) in the United States and the third most common cancer in both men and women. Nearly one million new cases occur each year worldwide, accounting for 9-10% of all cancers. The highest rates are found in Europe, the United States, Australia, and New Zealand; the lowest rates are found in India, South America, and the United Arab Emirates. Rural populations have lower rates than urban populations.
Causes of rectal cancer:
+ Rectal polyps:
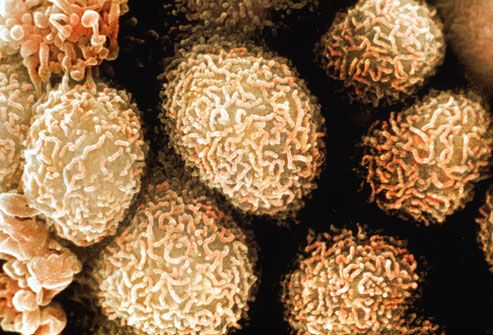
Polyps grow inside the colon or rectum. Most polyps are benign, but some can turn into colorectal cancer if not removed early. The two most common types of intestinal polyps are adenomas and hyperplastic polyps.

Hyperplastic polyps
These are normal polyps that form in the rectum or lower colon . They are small and have the lowest risk of becoming cancerous. According to the College of American Pathologists, hyperplastic polyps are the most common type of polyp and are most often found in people between the ages of 50 and 70. They grow slowly and continue to grow if not detected and removed by colonoscopy.
Tubular Adenoma
About 10% of all colon polyps are adenomas. Tubular adenomas are the most common type and can form anywhere in the colon. As they grow, they can lead to cancer, says a staff member at the Endoscopy Center. Tubular adenomas appear without causing any symptoms. If detected early by endoscopy, tubular adenomas can be removed before cancer cells have a chance to form.
+ Daily eating habits: The metabolism of animal fat along with eating foods low in fiber slows down the digestion of the colon, increasing the absorption of toxins.
+ Personal history of cancer: A person who has had colorectal cancer may develop colorectal cancer a second time. Additionally, women with a history of ovarian, uterine (endometrial), or breast cancer have a slightly higher risk of developing colorectal cancer.
+ Family factors: If you have a positive family history of colorectal cancer, you are more likely than others to develop the disease, especially if your relatives had cancer at a young age.
+ Lifestyle factors: People who smoke, or eat a diet high in red or processed meat and low in fiber have an increased risk of colorectal cancer.
+ Age factor: Colorectal cancer is more likely to occur in older people. More than 90 percent of people with this disease are diagnosed after age 50 and older.
Signs and symptoms of colorectal cancer depend on where the tumor is in the bowel, and whether it has spread to other parts of the body ( metastasis ). Early warning signs include: constipation , passing small, bloody stools, stomach cramps, loss of appetite , fatigue, unexplained weight loss, and nausea or vomiting in a person over age 50. Usually, these symptoms are not caused by cancer. Other health problems can cause some of these symptoms. Early stage cancer is often painless. While rectal bleeding or anemia are high-risk features in people over age 50, other commonly described symptoms include weight loss and changes in bowel habits, which are usually only concerning if associated with bleeding.
Measures to detect rectal cancer:
+ Sigmoidoscopy
Examine the rectum and lower part of the colon with a colonoscope.
Precancerous and cancerous growths of the rectum and lower part of the colon may be found and either removed or biopsied.
+ Sigmoidoscopy
Examination of the rectum and entire colon with a colonoscope. Precancerous and cancerous growths throughout the colon can be found and either removed or biopsied, including growths in the upper part of the colon, where they would be missed by a sigmoidoscopy.
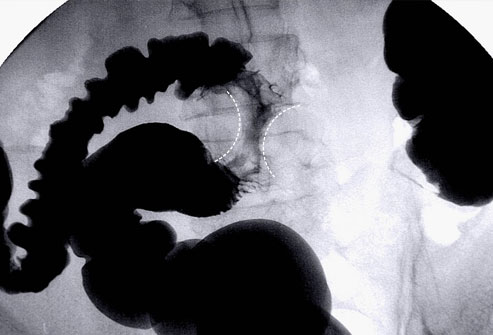
+ Barium enema
This procedure involves filling the colon and rectum with a white liquid (Barium) to enhance the X-ray images. Abnormalities (such as polyps) can be seen clearly.
+ Fecal occult blood test
Sometimes cancers or polyps cause bleeding, and the FOBT can detect small amounts of blood in the stool. If the test shows blood, then other tests are needed to find the source of the blood. Benign conditions (such as hemorrhoids) can also cause blood on this test.
+ Biopsy:
Doctors will take samples from any part of the rectum they suspect and study them under a microscope to determine whether it is cancerous.
Treatment :
+ Surgery:
Is the first choice in the treatment of rectal cancer. Surgery to resect the tumor-bearing rectum - end-to-end anastomosis or Miles surgery for cases of low rectal cancer. Currently, laparoscopic surgery is increasingly developed and has the same effectiveness as classic open surgery but has superior effectiveness in terms of aesthetics, reduces hospital costs and uses less pain medication.
+ Chemotherapy:
Helps improve patient survival and reduce the risk of disease recurrence after surgery. The most commonly used chemotherapy is 5FU, capecitabine, irinotecan and oxaliplatin. The FOLFOX or FOLFIRI ± Bevacizumab regimen is considered the first standard regimen applied by most oncologists.
+ Radiotherapy:
Effective in rectal cancer: helps treat the disease, reduce the stage of the disease, reduce tumor size, or palliative care radiotherapy.
In Europe, the five-year survival rate for colorectal cancer is less than 60%. In developed countries about a third of those with the disease die.
Survival rates are directly related to detection and the type of cancer, but are generally low for cancers that have symptoms, as they often grow quite quickly. Survival rates for early stage detection are about five times higher than for late stage cancer.
According to the American Cancer Society in 2006, more than 20% of people with colorectal cancer come to medical care when the disease is advanced (stage IV), and up to 25% of this group will have isolated liver metastases that are potentially resectable. Of this group, those who undergo resection have a five-year survival rate of one-third.